Americans spent $425 billion on prescriptions in 2015, a more than 12 percent increase from 2014. And the nation’s spending on medicines is forecasted to reach $610-640 billion in 2020. Adding to these costs is prescription abandonment due to unpleasant copay surprises at the pharmacy and the resulting medication non-adherence. Ten percent of people who abandon their prescriptions do so because of cost, and two-thirds of medication-related hospital admissions in the U.S. stem from medication non-adherence at a cost of $100 billion per year.1
A recent ORC International survey commissioned by Surescripts reveals that most physicians believe in the value of prescription price transparency to aid in making medication decisions.
This and other key findings are now available in our new report Physician Perspectives on Access to Patient Data.
Although 56 percent of physicians think that it’s a priority, only 11 percent report the ability to easily retrieve out-of-pocket medication cost information—a sizable disparity between importance and access that’s indicative of an opportunity to better serve physicians with the actionable patient intelligence that they want most.
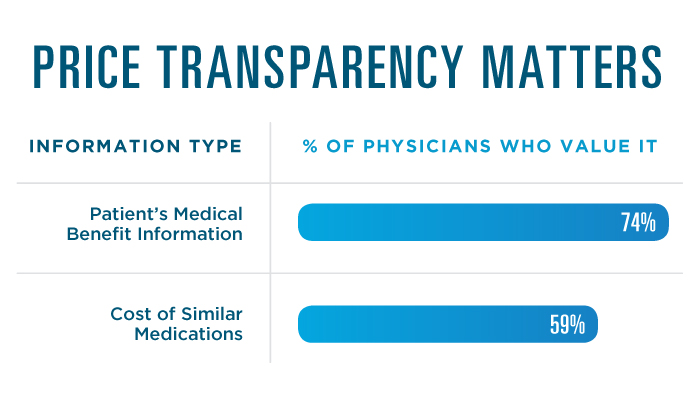
More than just nice to have, the majority of physicians believe that patients’ out-of-pocket costs should impact their prescribing decisions. Seventy-four percent think that it’s important to consider a patient’s medical benefit information before prescribing, and 59 percent want to be able to compare the cost of similar medications.
As prescription prices continue to change, the comfort of knowing the cost before the patient goes to the pharmacy will be increasingly vital to effectively fulfilling their care plan. For example, in 2009, Mylan’s two-pack EpiPen Auto-Injector was $100. By 2016, it was more than $600, demonstrating that today’s prescription price is likely not tomorrow’s. Price transparency at the point of care is and will be the key to keeping patients and their healthcare providers in sync and able to choose the most affordable treatment plan while maintaining proper efficacy.
According to the National Academies of Sciences, Engineering and Medicine’s Making Medicines Affordable: A National Imperative, “Hospitals, vendors of electronic health records, insurers, and professional societies should ensure that clinicians have readily accessible and routinely updated information regarding drug cost and efficacy to support sound prescribing decisions at the point of care. This information should include the relative clinical benefits of alternative treatment regimens and the relative financial costs of treatment settings to both patients and payers.”
Surescripts Real-Time Prescription Benefit integrated with Prior Authorization and E-Prescribing delivers patient-specific drug benefit and cost information—including therapeutic alternatives and their costs—within the e-prescribing workflow at the point of care.
This means that prescribers can see what a medication will cost their patient based on their specific health plan coverage and pick the most affordable medication that meets their therapeutic need. Once the most appropriate and affordable medication is selected, if an authorization is still required, it may be quickly completed during the office visit within the EHR workflow. It is then sent to the pharmacy, resulting in the patient leaving the doctor’s office confident in both the medication choice and the medication cost, knowing that it will be covered by their insurance.
“From research we've done at Express Scripts over the last several years, we've seen that about 15 to 16 percent of non-adherence is simply due to the patient not being able to afford their medication,” said Dr. Lynne Nowak, Vice President, Clinical and Provider Solutions at Express Scripts. “So being able to have that discussion at the point of care with the physician really helps at least answer if the patient's going to be able to afford the medicine when they get to the pharmacy, and the patients don't get that sticker shock and walk away and unfortunately abandon the script, which happens all too often … Combining the real-time prescription benefit information with prior authorization information, and the ability to do that prior authorization electronically is really transforming the entire physician experience with their patient.”
To learn more about the state of physician access to and need for actionable patient intelligence, download the report Physician Perspectives on Access to Patient Data.
1 "Adherence to Medication." The New England Journal of Medicine, August 4, 2005


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts
