Pharmacists are many things—counselors, medication experts and key members of a patient’s care team. And our ability to deliver safe and high quality care largely depends on the quality and accuracy of the e-prescriptions we receive. We need to be able to clearly understand the prescriber’s intent, and it’s even better if we can stay in our workflow while we’re at it.
Usually, we can make logical assumptions about what the prescriber originally intended when they wrote a prescription, and we can supplement any gaps by using other information or common sense. However, in some situations, quality issues in the prescription necessitate callbacks to prescribers for clarification, or we risk medication errors and patient safety.
I often wonder exactly where that fine line should reside. When should pharmacists feel safe enough to make certain logical assumptions or supplement gaps themselves in interpreting and filling a prescription? When should we decide that the information is too ambiguous to clearly discern the prescriber’s original intent, and that it’s too risky to proceed without clarification?
This boundary will vary from one pharmacist to another. But there is one thing I know for sure. As an industry, we should seize any and all opportunities to reduce the avoidable ambiguity that forces disruptive decisions or causes unnecessary risks. When we have to spend additional time trying to decipher unclear information using logical assumptions or leave workflows to make calls for clarification--and interrupt prescribers in the process—it negatively impacts all of us, and most importantly, the quality of patient care.
Over the past several years, I have witnessed significant growth in e-prescribing, which today is standard practice for most physicians, especially given the vast amounts of incentives and legislative mandates in place to promote its meaningful use. The benefits of adopting e-prescribing are well established and have significantly improved the quality and efficiency of patient care as compared to traditional paper prescriptions.
But this technology is only as beneficial as its appropriate utilization. When e-prescriptions are sub-optimally written and transmitted with inappropriate or unclear information, not only are e-prescribing’s benefits lost, but new challenges and risks are also introduced. Hence, there are significant quality improvement opportunities that we can seize in partnership to ensure e-prescribing’s value is fully realized.
The patient directions, or Sig (signetur), is one of the most critical elements of a prescription. It’s also one of the most prone to quality challenges due to the wide variance in styles when prescribers use free-text. This coupled with the differences in Sig creation tools within the several hundred available e-prescribing software applications makes for a precarious situation for everyone.
Here is an example of a confusing Sig that model Chrissy Teigen publicized on Twitter last year.
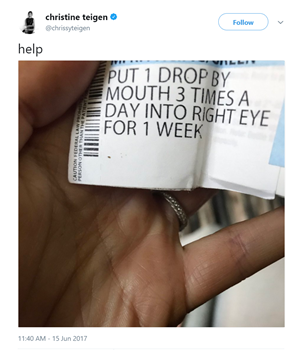
Confusing directions like these that contradict themselves or conflict with the prescribed medication are just one of many quality issues with Sigs, exemplifying why improvements are needed. As a clinical informatics pharmacist, I’ve also encountered Sigs with inappropriate dosing information for injectable medications. For example, a prescription for anti-diabetic drug Victoza had the Sig “Inject 1.8 mls sub-q every day” instead of 1.8 mg—essentially instructing the administration of a dose six times the appropriate amount. But that’s only if this amount was even possible for patients to administer, since the injector only displays units of milligrams.
Other trends I’ve observed involved incomplete directions. Many were missing the elements essential for unambiguous understanding of intended medication administration, e.g. Sigs for prednisone that state simply “Take by oral route.” Furthermore, there is frequent misuse of the Sig data field entirely, with information like “Please enter as generic Alendronate” or “Dx:250.00,” which are not patient directions at all.
In our recently published study in the Journal of Managed Care and Specialty Pharmacy, we reviewed a nationally representative sample of ambulatory e-prescriptions to assess the variability in how Sigs conveying the same core concept are written. At times, we observed variations as extreme as 800 permutations of a single concept like “Take one tablet by mouth once daily.”
We also identified and categorized the types of quality issues present in Sig free-text that can pose significant workflow disruptions or patient safety risks.
We found that more than one in ten e-prescriptions had Sigs containing a quality issue with the potential to cause confusion or workflow disruption at the pharmacy. Considering the fact that more than one billion e-prescriptions a year flow through Surescripts, or nearly five million daily, these quality issues and the resulting inefficiencies add up quickly. It means that every day, more than ten percent of Sigs require manual intervention or callbacks, costing the industry additional time and money and potentially impacting care quality.
Interestingly, the most frequently observed quality issues were related to incomplete Sigs missing either relevant dosage or administration frequency/timing information—two components essential to the Sig being clear and actionable, and to the pharmacists avoiding the need to make assumptions or phone calls to prescribers.
Our evidenced-based insights from the study allow us to recommend enhancements to the design and functionality of electronic health records (EHRs) and e-prescribing applications, as well as inform our Critical Performance Improvement program, which brings together participants from across the Surescripts Network Alliance to perfect e-prescribing. Our recommendations include improving prescriber end-user training and prioritizing the adoption and implementation of available features in the current e-prescribing standard, like the structured and codified Sig format that can help address many quality issues. Structured and codified Sig is just one step on the path to reaching zero-error e-prescribing—a lofty goal but one that is within our reach. Achieving it requires industrywide support, adoption of best practices and above all, our shared commitment to keeping patients safe.
As I examine all of the available e-prescribing tools and technology options, including the upcoming version of the NCPDP SCRIPT standard and the enhancements to the schema, I am encouraged by the direction our industry is moving. Together, we are refining and expanding structured and codified Sig functionalities to capture and convey prescriber intent as closely and accurately as possible. I’m optimistic that the future is indeed bright as an ever-increasing number of our technology partners choose to embrace these functionalities—whether they’re new or previously existing and still evolving—and leverage them to their optimal potential. I am confident that the available tools, when used in tandem with the best practices derived from our study, will reduce the need for assumptions or workflow interruptions, improve overall prescribing experiences for prescribers and pharmacists, and ultimately enhance patient care.
The partnership between pharmacists and prescribers is key to increasing quality, enhancing safety and lowering costs. We need robust systems and technologies to minimize human error. So utilizing the tools we have available today in the optimal manner is key to ensuring complete, clear and accurate e-prescriptions, every time.
Like all big healthcare challenge, it takes a network. Want to join us in perfecting e-prescribing and improving healthcare for all? Learn more about The Surescripts Network Alliance and our Critical Performance Improvement program.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts