
See why we’re trusted by healthcare organizations across the country.
Learn more
William J. Mayo, MD, (“Doctor Will”) said, “The best interest of the patient is the only interest to be considered, and in order that the sick may have the benefit of advancing knowledge, union of forces is necessary.”
As an innovator in the rapidly expanding specialty prescribing space, I have spent time with a number of patients and providers who are working together to treat serious illnesses.
I invest myself in this work in the name of every American patient I see in the headlines who is battling both their disease and their insurance company. And I bring my expertise to bear with passion and urgency in the name of my loved one who is bravely facing a very serious diagnosis.
Collectively, these experiences have made clear to me a resounding sentiment: We urgently need a streamlined, automated process for prescribing specialty medications.
When a patient is diagnosed with an aggressive form of cancer, they need to start their specialty medication immediately. But the process today for doing so is lengthy, and it’s often the patients with no time to waste who are left waiting.
According to our recent survey, most prescribers don’t have digital access to trusted information about:
And the costs of specialty medications can be high. In 2017, the average annual retail cost of prescription drug therapy for a single specialty drug was $78,781 per year—almost $20,000 more than the U.S. median household income of $60,336.
With branded specialty medications projected to surpass half of all medication spending in the U.S. by 2022, prescribers need to be able to compare their selected medication with therapeutic alternatives that may be more affordable for their patient.
Here’s a real-world example.
Earlier this year, I listened as a participant at an event hosted by the National Council for Prescription Drug Programs (NCPDP) shared her experience. She was prescribed a new specialty medication and sent to her typical pharmacy.
When she arrived, she discovered that her annual out-of-pocket cost for the medication would be $44,000. For a number of reasons, it took months—not days or weeks—to get started on her medication.
But solutions to this problem do exist. EHR-integrated drug cost information is already saving patients thousands of dollars at the pharmacy.
Take a look at a typical specialty patient enrollment form:
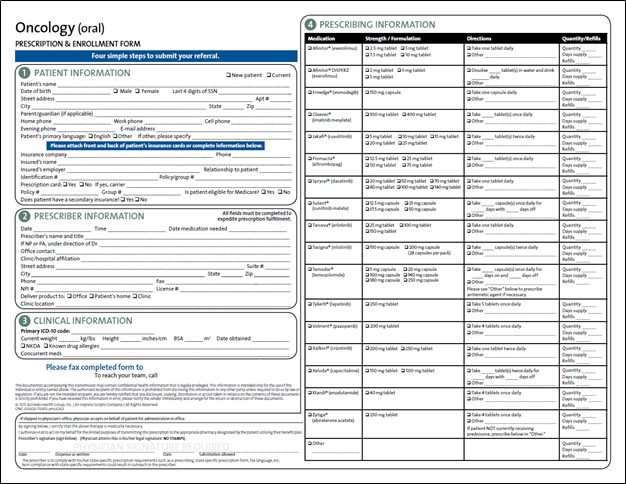
These highly detailed documents are required, but often cause a lot of back-and-forth between the prescriber and the pharmacy.
Here’s the bottom line: According to a recent customer interview, the best case scenario for completing the specialty patient enrollment form with the manual workflow is 3-5 days.
Compare this to the 90 minutes it takes the electronic workflow to auto-initiate, populate and return the same information—but completely and accurately on the first attempt. And this timeframe will only shorten as the technology gains traction.
Specialty medications and the conditions that they treat are already complex. Yet today, doctors who give patients a tough diagnosis can also offer them hope in the form of an innovative treatment plan, thanks to the incredible progress made by medical science.
I believe that nothing should stand in the way of that progress, nor the hope that it offers. We can knock down the barriers created by paper forms, missing information and outdated workflows with solutions that provide access to the right information at the point of prescribing.
With these tools in hand, healthcare providers and patients can work together to choose the most affordable and appropriate medication, and be assured that it was successfully authorized by the patient’s benefit plan at the point of care. And when coupled with an automated prior authorization and specialty patient enrollment process, we can reduce the time patients are waiting before starting their much-needed specialty therapy.
Learn more about prescription price transparency and electronic prior authorization.