Did you know that 25% of the time, if a prescription copay is more than $50, patients won’t fill it? The connection between medication cost and medication adherence is undeniable. And so is the dependency between high-quality eligibility and formulary data at the point of care and the prescriber’s ability to choose the best possible medication for their patients, both clinically and economically.
As Practice Lead for PBM Services at Point-of-Care Partners, I recently had the pleasure of joining Andrew Mellin, M.D., Vice President and Chief Medical Information Officer at Surescripts, for a discussion guided by Jennifer Covich Bordenick, Chief Executive Officer of eHealth Initiative & Foundation. We shared our insights on realizing the power of patient benefit data delivered to the point of care. Now more than ever, it’s critical for our industry to have an understanding of this must-have technology, and to seize every opportunity to enhance the care experience for prescribers and their patients.
With complete and accurate eligibility, formulary and benefit data as the foundation, a range of downstream interactions are made possible. And tremendous value is created when we give prescribers the ability to conduct a real-time benefit check, an electronic prior authorization, or an automated and streamlined enrollment for specialty medication for patients who simply can’t afford to wait. Benefit information also extracts more value from e-prescribing, which when used with benefit information is associated with as much as a 20% increase in first-fill medication adherence.
As Dr. Mellin explained, “When we talked to prescribers, 83% of them said they think about this benefit data as they prescribe. Two-thirds of them said they will change their medication decision if there is a different option at a better preference level on the formulary. So, this is something prescribers think about, it’s essential for medication adherence, and it’s truly available for virtually every patient in the country.”
A 2019 survey of prescribers showed that benefit insights help them optimize prescriptions in several ways, and the vast majority would indeed consider changing a prescription. 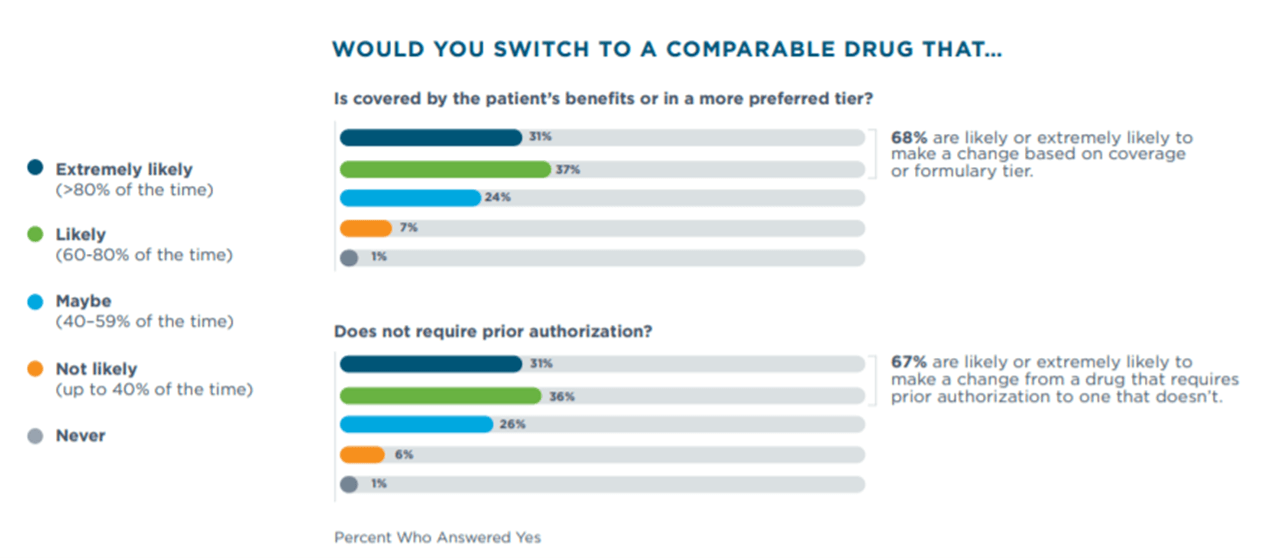
Coming Soon: Formulary and Benefit File Updates (Version 5)
The National Council for Prescription Drug Programs (NCPDP) has formed a task group devoted to enhancing the formulary and benefit file in a number of ways. Designed to ensure that the industry can realize the full value of high quality formulary and benefit data, here are a couple of enhancements that are of particular significance, and will be named along with several others in an upcoming rule from the Centers for Medicare & Medicaid Services (CMS).
- Indication-based formulary to allow a payer to communicate to the prescriber if the drug is covered for a specific diagnosis and not another.
- Specialty drug support to allow a payer to indicate for the prescriber when a drug is classified as specialty, and alert them beforehand of the need for more information for the pharmacy to dispense the drug.
- File expiration date to ensure that prescribers have the most recent eligibility files and can trust the information.
Together, we’re improving quality and forging a deeper understanding of why it matters—not only for eligibility and formulary, but the downstream impact it has on every facet of healthcare, and most importantly, the patient. Accurate eligibility and formulary data helps ensure patient safety, improves time to therapy and enhances patient care and outcomes.
Learn more about Eligibility & Formulary and subscribe to Intelligence in Action to stay informed and engaged with the issues that impact healthcare.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts





