As patients make the journey from their doctor’s office to their pharmacy, a lot can go wrong behind the scenes that ultimately delays treatment and drives up healthcare costs. According to the IQVIA report on medicine use and spending in the U.S., commercial health plans see abandonment rates of more than 31% when the out-of-pocket cost of a prescription is $50 or more.
Thankfully, pharmacists and their support staff can take action to help patients receive and adhere to their needed medications. They act as a tremendously capable safety net, solving problems and consulting with patients while balancing multiple priorities and supporting the goals of both prescribers and health plans. But the pharmacy’s critical role also means that their daily operations are profoundly impacted when the patient journey slows or comes to a halt. And it’s often because the question of a medication’s cost or coverage—and whether there are more affordable alternatives—can’t be answered quickly and easily.
Pharmacy Perspectives on Prescription Cost and Coverage Barriers for Patients
Could the right technologies make it faster and easier for pharmacies to remove these barriers for patients? We surveyed pharmacy staff to find out.
Our recent survey of 230 pharmacists and technicians highlights the top issues that are disruptive to pharmacy workflows and get in the way of patients receiving the right medication at a cost they can afford. The survey responses identify how technology can deliver in-the-moment insights that let pharmacists get off the phone, stop “sticker shock” in its tracks, improve adherence and patient safety, and more easily operate at the top of their license. 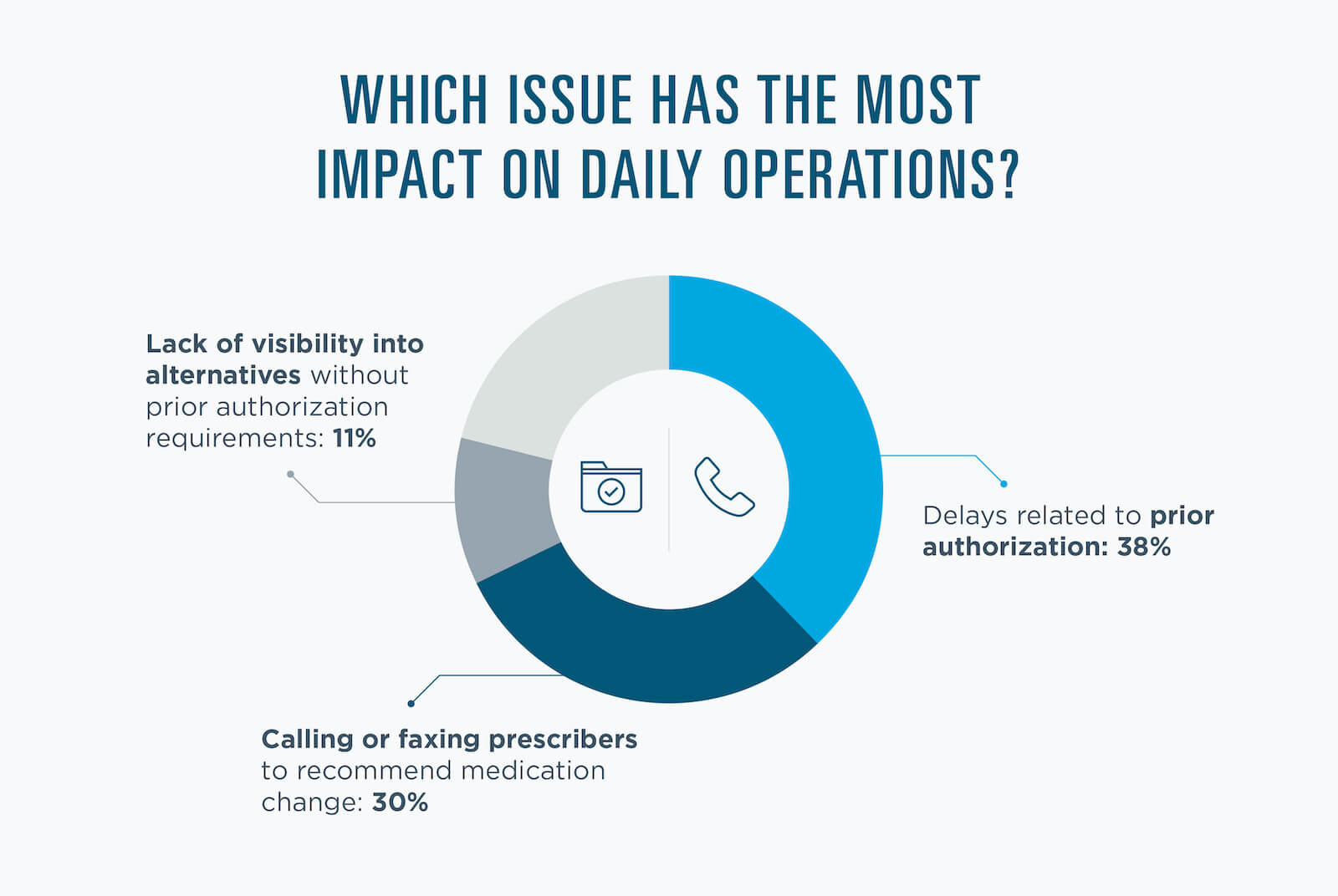
As an industry, and in the best interest of patients, it’s time to help pharmacists get off the phone with benefit plans and get real-time insights they need into cost and coverage details, enabling them to deliver unlimited value with the right tools in hand to light their way.
“It’s competing demands,” explains Surescripts Clinical Informatics Manager Larry King, whose retail pharmacy experience began as an intern and pharmacist in New York City. “In an inherently busy retail environment, pharmacists have so many critical boxes to check. Wherever we can save them time—too much of which is spent trying to understand the patient’s drug benefit and out-of-pocket cost—it means happier patients who trust their pharmacy and keep coming back.”
Surescripts is building the future of prescribing through innovations that enhance the entire prescribing process to accelerate time to fill and improve adherence. Surescripts Real-Time Prescription Benefit empowers pharmacists to proactively resolve price and process concerns, creating an exceptional experience for patients and a better workflow in the pharmacy. With the power to address cost concerns and prescription changes within their workflow, pharmacists can prevent abandonment and restocking that often result from prescription delays.
View the report and get more insights on how prescription price transparency helps pharmacists knock down the barriers that stand between patients and their medication.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts