When it comes to the state of our health in the U.S., the playing field is anything but level.
Study after study has shown that life circumstances, such as access to adequate food, education and healthcare, have a bigger impact on our health than our genetic makeup.
In other words, our healthcare destiny may depend more on our ZIP code than our genetic code.
Take Chicago, for example. According to Root Causes of Health, people who live in the heart of downtown (aka “the loop”) have an average life expectancy of 83 years. That’s 14 years longer than people who live just three train stops away in Washington Park, whose life expectancy is just 69. This life expectancy gap is larger than the one between the U.S. and Honduras, one of the poorest countries in Latin America with one of the world’s highest murder rates.
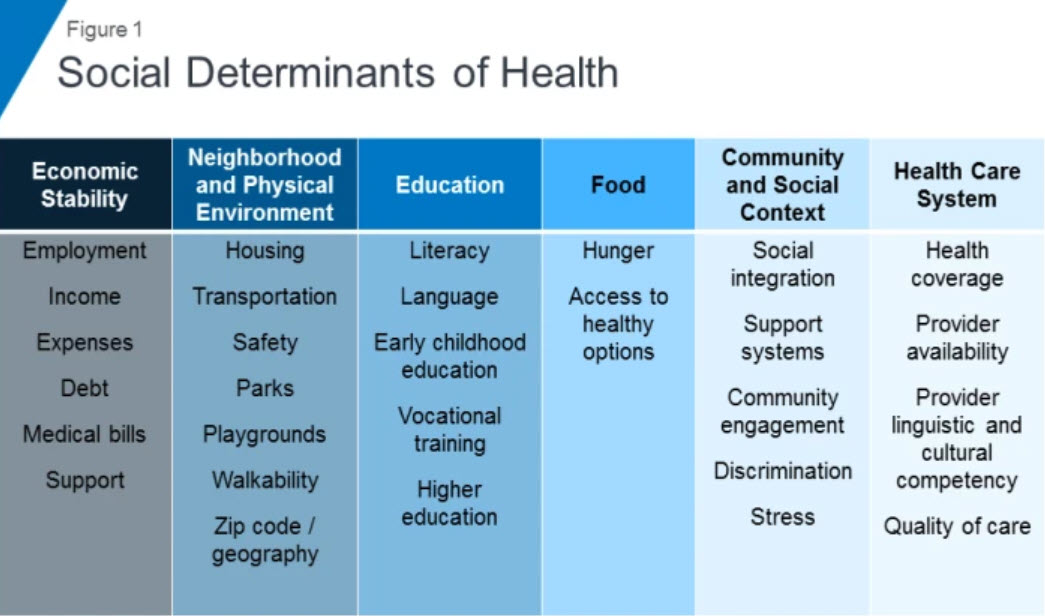
The Kaiser Family Foundation defines these social determinants of health as "factors like socio-economic status, education, neighborhood and physical environment, employment and social support networks, as well as access to healthcare."
A study of physician attitudes about the social determinants of health revealed that 66% of physicians surveyed believe assistance with transportation arrangements helps patients. According to Social Determinants of Health: From Insights to Action, for many, the failure to take medications as prescribed, or medication non-adherence, is often tied to transportation challenges. Research published in the Annals of Internal Medicine and referenced in the whitepaper above suggests the cost of medication non-adherence to the U.S. healthcare system is between $100-289 billion a year.
How Health Plans are Taking Action
Understanding and navigating a patient’s healthcare destiny and addressing social determinants of health are critical for health plans looking to ensure appropriate and meaningful patient care, particularly when it comes to medication adherence. More than eight in 10 insurers are currently integrating social determinant of health factors into their member programs.
WellCare found that “Connecting patients with social services to address social determinants of health generated a double-digit reduction in healthcare spending. The study reported an additional 10% decrease in healthcare costs, equating to more than $2,400 in savings per person per year for Medicare and Medicaid members who were successfully connected to social services compared to a control group of members who were not.”
According to a Moody’s analytics report released by the Blue Cross Blue Shield Association, Understanding Health Conditions Across the U.S., for some common chronic conditions like diabetes and hypertension, social determinants drive larger differences in health impacts. For instance, diabetes “strongly correlates with unemployment, less education and obesity.”
But this puts physicians, nurses, pharmacists and others who are already overburdened in a tough spot. They need time with patients to uncover and address the social determinants of health. But it’s time they simply don’t have, due in large part to manual processes that take too much time and effort away from patient care.
Technology Gives Patients and Providers More Time to Talk
By digitizing manual processes, like processing prior authorizations or delivering price transparency at the point of prescribing, health plans can redirect resources to supporting important community programs that address the social determinants of health of their members. Improved programs mean a better prescriber and patient experience.
Two powerful technologies converge to support this evolution: Real-Time Prescription Benefit and Electronic Prior Authorization.
With the right information in their electronic health record (EHR), the prescriber can review therapeutic alternatives that may be less expensive or more accessible—a 90-days supply at a lower out-of-pocket cost via mail order, for example. And they can avoid a prior authorization—which is often another barrier to medication adherence due to patient wait time—and choose an option that doesn’t require one. Or if prior authorization is unavoidable, they can initiate it electronically from their EHR rather than via phone and fax machine, and get a response back in minutes rather than days.
Ultimately, they can send their patient out the door with confidence knowing that their medication will be ready, and what they’ll be asked to pay at the pharmacy is the exact out-of-pocket cost that their doctor shared with them during the office visit.
Members benefit from cost alternatives being displayed in the provider workflow at the point of care. This creates a clear and straightforward patient-provider experience in which members get all the information they need during the appointment. They leave knowing what the drug is and how to take it, what it will cost and that it’s covered and authorized.
At the pharmacy, the member receives the same information their doctor told them. With the administrative work managed seamlessly in the background, the steps to begin and maintain therapy are clear, consistent and accessible.
For prescribers, spending less time ordering a prescription means more time to talk with their patient. By freeing up time from figuring out what’s on formulary or initiating a prior authorization, prescribers can uncover social determinants of health that may prevent their patient from following their medication therapy, have an impact on their recovery or hinder the maintenance of their diagnosis in other ways.
Together, we can use technology to remove barriers at the point of care while improving medication adherence—which is especially key for members who struggle with access to transportation or economic stability. A future where healthcare providers have the information they need to gain a deeper understanding of their patient, and all the factors that may support or undermine high quality care, is well within our reach.
Visit our Benefit Optimization page to learn how to free up resources to focus on social barriers to member care to improve outcomes and member satisfaction. Learn more about price transparency and how real-time benefit tools and prior authorization can have an immediate and positive impact on healthcare cost, quality and safety.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts