In a recent survey by America’s Health Insurance Plans (AHIP), health insurance providers pointed to the automation of the prescription prior authorization process as a critical area in need of meaningful reform. Specifically, 84% of health plans identified automating the prior authorization process as one of the biggest opportunities for improvement.
I spoke with Kate Berry, Senior Vice President of Clinical Affairs and Strategic Partnerships at AHIP, about the study, which aimed to get a better sense of where, when and how prior authorization is being used. AHIP conducted the survey between September and December of 2019 and their sample included 44 health plans with commercial enrollment of at least 50,000 lives, for a total of 109 million enrollees.
The survey findings clearly show how necessary prior authorization is in improving quality and safety for patients – as well as improving health care affordability for everyone. In fact, a vast majority of health plans reported positive impacts from prior authorization programs in terms of quality of care, affordability, and safety.
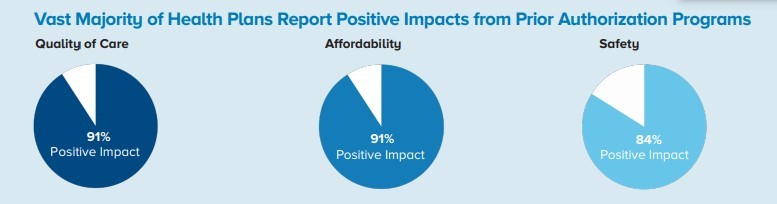
“Key Results of Industry Survey on Prior Authorization,” AHIP, accessed July 31, 2020
Yet despite its impact and grounding in evidence-based resources, AHIP’s survey found electronic prior authorization is still used selectively by providers.
Fifty-eight percent of plans said the most common barrier to automating prior authorization programs is that the provider does not use electronic health record (EHR) software that enables electronic prior authorization. In a separate study, the American Medical Association found that 46% of prescribers submit requests by fax, and 60% require a telephone call.
When I asked Kate how the industry can work together to overcome these barriers to prior authorization automation, she pointed to collaboration.
“There is no doubt that moving toward industry-wide adoption of electronic prior authorization requires a collaborative effort among providers, health insurance providers, health IT companies, health systems and PBMs,” she explained. “We must all work together to accelerate the use of national standards for electronic prior authorization and the exchange of clinical attachments.”
Groups across the healthcare industry are working to increase safety, lower costs and ensure quality care for patients by identifying strategies to improve outcomes. And AHIP is doing their part. AHIP’s new Fast-Prior Authorization Technology Highway (Fast PATH) initiative is a demonstration project designed to show the impact of automation on the prior authorization review and determination process. The effort leverages Surescripts and Availity to speed prior authorization requests, responses, and information exchange.
“Greater use of electronic prior authorizations will improve efficiency by minimizing phone calls and faxes, improve quality by reducing the time to treatment and improve overall care and safety by tying prior authorization requirements to evidence on safety and effectiveness,” Kate shared.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts






