As American healthcare faced the second year of the COVID-19 pandemic, the “new normal” still involved a great deal of change.
The lives and needs of the patients we serve certainly changed. Research now confirms that COVID-19 has not only caused nearly 1 million deaths in the U.S. directly, but increased deaths from many other conditions worsened by disruptions in routine and preventive care. It’s more critical than ever for healthcare professionals to know their patients’ histories and proactively monitor their health.
Roles in healthcare changed, too. Hospitals stretched their resources as COVID-19 surges filled beds. Telehealth and remote work meant that more of us did our jobs at a distance, heightening the need for fast and efficient communication channels. Pharmacies administered tests and vaccinations on top of their normal care duties.
How are American healthcare professionals and organizations responding to all this change? Our 2021 National Progress Report makes one answer clear: They’re sharing more trusted health intelligence.
2021 National Progress Report
In 2021, U.S. healthcare professionals shared health intelligence to make care better, safer and less costly. Explore the progress we made together.
Here are five major trends I see in the data we’re releasing today.
Interoperability across healthcare is gaining even more momentum.
Technology is supporting pharmacies’ central role in today’s care landscape.
Clinicians are solving for medication affordability and adherence up front.
Shared intelligence is simplifying specialty medication workflows.
E-prescribing is improving safety and efficiency for even more prescriptions.
Above all, this year’s National Progress Report demonstrates nationwide momentum toward interoperable, digital health intelligence sharing. In 2021, the Surescripts network helped inform billions of healthcare decisions and conversations. More connected healthcare professionals and organizations gained access to more trusted intelligence for the patients they serve.
The capacity to exchange health data alone is not enough to deliver on the promise of interoperability. Care teams need meaningful, consumable intelligence delivered at the right moment in the patient’s care journey.
While there’s certainly more work to do, this is already happening at scale. We’re hearing stories from care management teams who are using new technologies to proactively gain insight into medication adherence for thousands of patients with diabetes, hypertension and high cholesterol. They’ve seen adherence scores rise—which helps set them up for value-based care success, too.
The pandemic introduced its own new interoperability demands, making clear just how many different hands it takes to keep patients healthy. Technologies like Direct messaging strengthened connections among hundreds of thousands of individuals and organizations, including public health agencies that gained a new digital channel to receive case reports.
Leveraging technologies like this, healthcare professionals of all kinds are communicating more efficiently and accessing information more easily. Ultimately, the Surescripts Network Alliance is helping them understand patients’ health much faster in a healthcare system where few care teams have time to spare.
Few places were as busy as a typical American pharmacy in 2021. Pharmacies faced opportunities to play an even larger role in patient care, but they also experienced severe staffing shortages.
To stay on top of it all, they needed technologies that would keep them connected to other care providers without having to step away from the counter to place phone calls, leave messages or send faxes. In 2021, the Surescripts Network Alliance supported them in many different ways, including giving them an automated way to report vaccinations to patients’ primary care providers.
As pharmacists became key players in the nation’s pandemic response, they still needed to fill prescriptions quickly and safely. Network participants made that simpler with continued improvements to prescription accuracy, safety and efficiency throughout the year, which added up to a 10% increase in Quality Index Score across the network.
Meanwhile, greater adoption of CancelRx alerted pharmacists to more discontinued prescriptions without taking them out of their workflow. RxChange growth meant more pharmacists could reach out to prescribers electronically to initiate prior authorization or suggest a more affordable therapeutic alternative—and receive replies in the same workflow. The RxChange response rate rose eight percentage points in 2021.
Workflow improvements like these are helping pharmacists meet the demands of their expanded role with less administrative burden and burnout.
Pharmacists and prescribers are very familiar with the relationship between a prescription’s out-of-pocket cost and the patient’s ability to adhere to their therapy. With virtually all U.S. prescribers served by electronic health record vendors that have implemented or plan to implement Surescripts Real-Time Prescription Benefit, it’s now possible to envision a world where clinicians can tell every patient how much their medication will cost and discuss any concerns up front.
That removes a significant risk to adherence and helps everyone feel more confident in their course of treatment—especially considering that 45% of Americans report that the COVID-19 pandemic has increased their worries about prescription drug costs. With fewer phone calls to benefit plans and prescriptions to rework, it’s easier for prescribers and pharmacists to deliver a better patient experience.
Along with greater transparency and efficiency, prescription benefit intelligence delivered meaningful savings in 2021: $36.68 per average prescription, to be exact. Considering that the average person in the U.S. fills about 12 prescriptions per year, that can add up to hundreds of dollars annually.
That figure rises to a remarkable $264 per prescription in one important area: specialty medications.
Innovation is moving quickly in the specialty medication space, and for good reason: Specialty medications now account for more than half of medicine spending in the U.S. For patients with serious or chronic conditions, a complex process can delay treatment and worsen symptoms.
It takes an extraordinary amount of collaboration to bring patients these essential medications. Specialty pharmacies and hubs stand ready to assist, but only if prescribers can easily share information with them.
That became possible for the clinicians who gained access to Specialty Patient Enrollment and Specialty Medications Gateway in 2021. These technologies automate the specialty prescribing and fulfillment process by gathering necessary clinical information so that pharmacists can fill prescriptions and hubs can initiate patient support services sooner.
When one specialty pharmacy implemented Specialty Medications solutions, they improved average time to fill by two days and dispense rate by 14%—while eliminating nearly half of the calls they’d been making to prescribers for missing clinical data.
In an era when some healthcare encounters take place entirely online, paper prescriptions have become nearly obsolete. Approximately 100,000 additional prescribers recognized that and began using E-Prescribing in 2021, joining virtually every pharmacy.
Electronic prescribing easily integrates with other technologies to help make the entire medication experience more efficient, even when additional steps such as prior authorization are required. America’s Health Insurance Plans conducted a study that found implementing electronic prior authorization reduced median wait time for a decision by more than two-thirds.
E-prescriptions aren’t just more efficient—they’re safer. Standardized data elements help create prescriptions that are less likely to contain conflicting or confusing information. Additional safety gains come from reducing the risk of fraud and making it easier to spot misuse, a continuing concern amid an opioid overdose crisis aggravated by the pandemic.
Federal and state governments have both emphasized the importance of this tool for public health. A Centers for Medicare & Medicaid rule requiring that Part D providers use Electronic Prescribing for Controlled Substances (EPCS) took effect at the start of 2021. And as of 2022, three-quarters of the U.S. population lives in states with legislation permitting or requiring e-prescribing for some or all prescriptions.
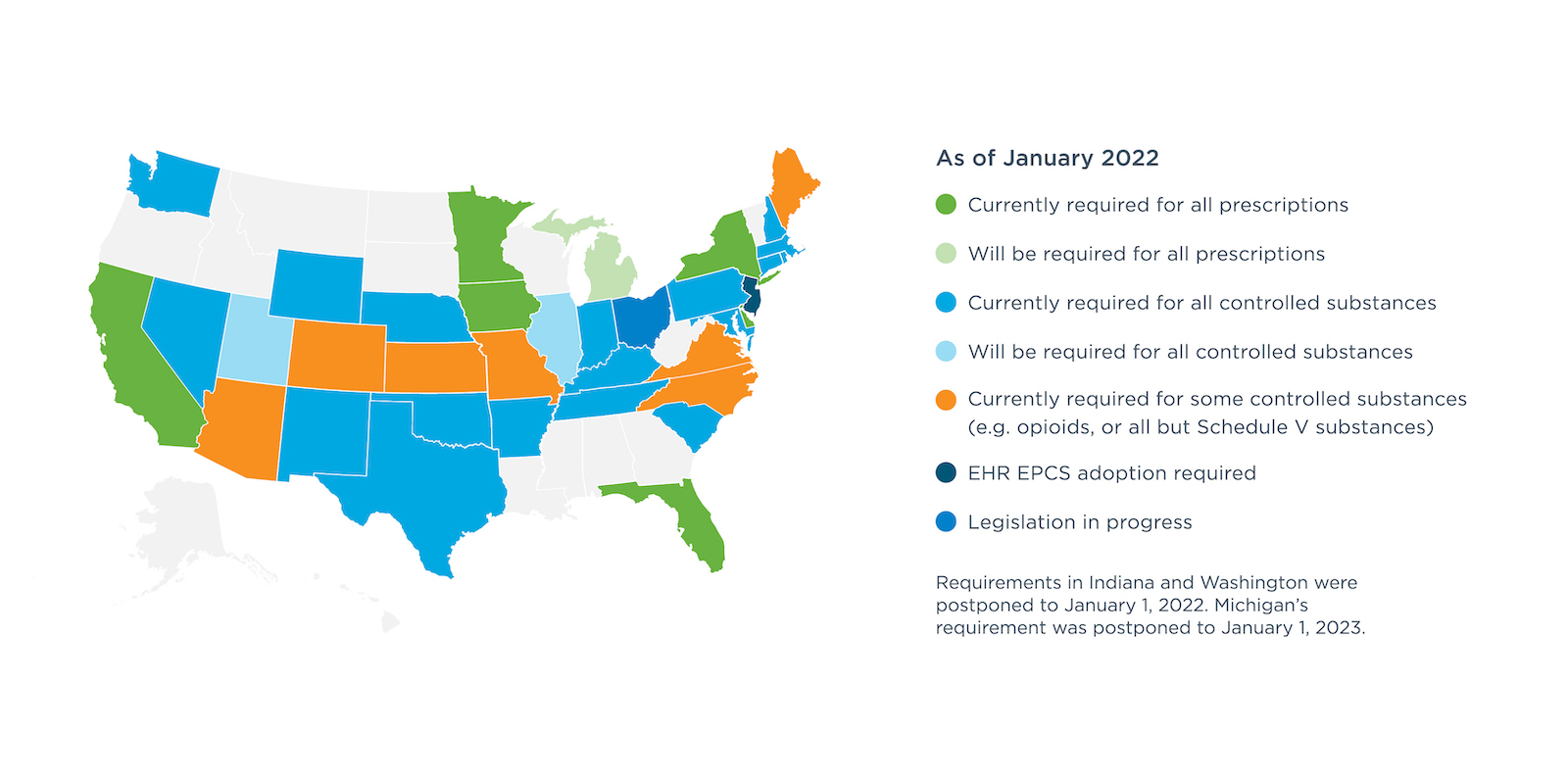
Looking back at the progress we’ve made on areas like EPCS as a nation, it’s inspiring to see how far we’ve come in just a few short years.
It gives me confidence that in a few more years to come, we’ll be equally struck by the progress we’ve made toward solving challenges like the complexity of interoperability, specialty prescribing, medication affordability and adherence.
I have that confidence because I’ve seen what we can do together amid a once-in-a-lifetime pandemic. On every page of this year’s National Progress Report, I see the momentum the Surescripts Network Alliance is building toward a better, safer, less costly future for American healthcare.
2021 National Progress Report
In 2021, U.S. healthcare professionals shared health intelligence to make care better, safer and less costly. Explore the progress we made together.


 Dean Riggott Photography
Surescripts
Dean Riggott Photography
Surescripts






